They’ve been visiting our clinic for a few months now, parents of a child with Glutaric Aciduria Type 1 (GA1), a rare metabolic disorder that can lead to irreversible brain damage if not managed carefully.
I met them for the first time on a relatively light clinic day. There wasn’t the usual rush, so I had time to go beyond the charts. I asked them where they were from, what work they did, and who was helping them at home. I don’t always get to do this often, as the crowd and chaos don’t allow it.
And that’s when the conversation turned. They used to live in a joint family. After the diagnosis, things changed. Slowly, quietly, they were left alone, not through arguments or dramatic exits, but through the absence of support, warmth, and shared responsibility. The unspoken weight of a genetic disorder had settled over the house, and one by one, others stepped away.
The isolation of families caring for a child with a rare genetic disorder is rarely about cruelty. It’s more often rooted in fear, stigma, and societal pressure, all of which run deep in traditional Indian households. In joint families, where collective reputation often outweighs individual struggles, a child with a chronic or inherited illness can become a silent source of anxiety. There’s a fear that having a “genetic condition in the family” will impact future marriage alliances, not just for the affected child, but for cousins, siblings, even extended relatives. Health conditions are whispered about in matrimonial circles, and families often preemptively distance themselves to “protect” their own children’s prospects. There’s also the ingrained idea that a sick child is somehow the result of someone’s “bad genes” or misfortune, leading to subtle blame, usually directed at the mother. Finally, the reality of long-term caregiving: hospital visits, dietary management, special schooling, and financial strain make some family members quietly back away, not out of hatred, but because they never wanted to shoulder the responsibility in the first place. The result? The parents, especially the mother, are left alone, not just physically, but emotionally and socially, carrying a burden that was never meant to be theirs alone.
The mother now handles the child’s feeds, therapy, and emergencies by herself. The father works longer hours. They never complained. But in that quiet room, I could sense the exhaustion and grief they’ve learned to carry.
They are both young, younger than me in fact, and perhaps that’s why I felt something shift inside me. We could have been classmates or friends from the same college batch. But life had placed them here, in a story far more demanding.
Then, they told me they were planning another pregnancy. I explained the recurrence risk of 25% as the disease is autosomal recessive, and the options for prenatal diagnosis through chorionic villus sampling (CVS). We discussed the timing, the logistics, and the need for mutation testing.
They listened. Took it all in.
Weeks later, they returned; this time, the mother was pregnant. We did the NT/NB scan at 12 weeks. Everything looked fine. We offered chorionic villus sampling (CVS) for early prenatal diagnosis. They chose to go ahead with the test. The CVS result was negative. The mother smiled, not with celebration, but with relief. For once, the weight in the room felt lighter.
Reflection
Sometimes, we don’t do anything extraordinary in clinic. We don’t make a diagnosis or change a treatment plan. We just listen. Ask the right question on the right day. And we get to witness something honest and raw.
A rare genetic disorder can isolate families in ways we don’t always see on the EMR. It can shrink their world. It can make them feel like they are the only ones carrying something no one wants to even acknowledge.
I didn’t change the course of their story. I just happened to be present at one of its quieter turns. And maybe, in that moment, that was enough.
Join Our Google Group
Join our google group and never miss an update from Gene Commons.
Join Google Group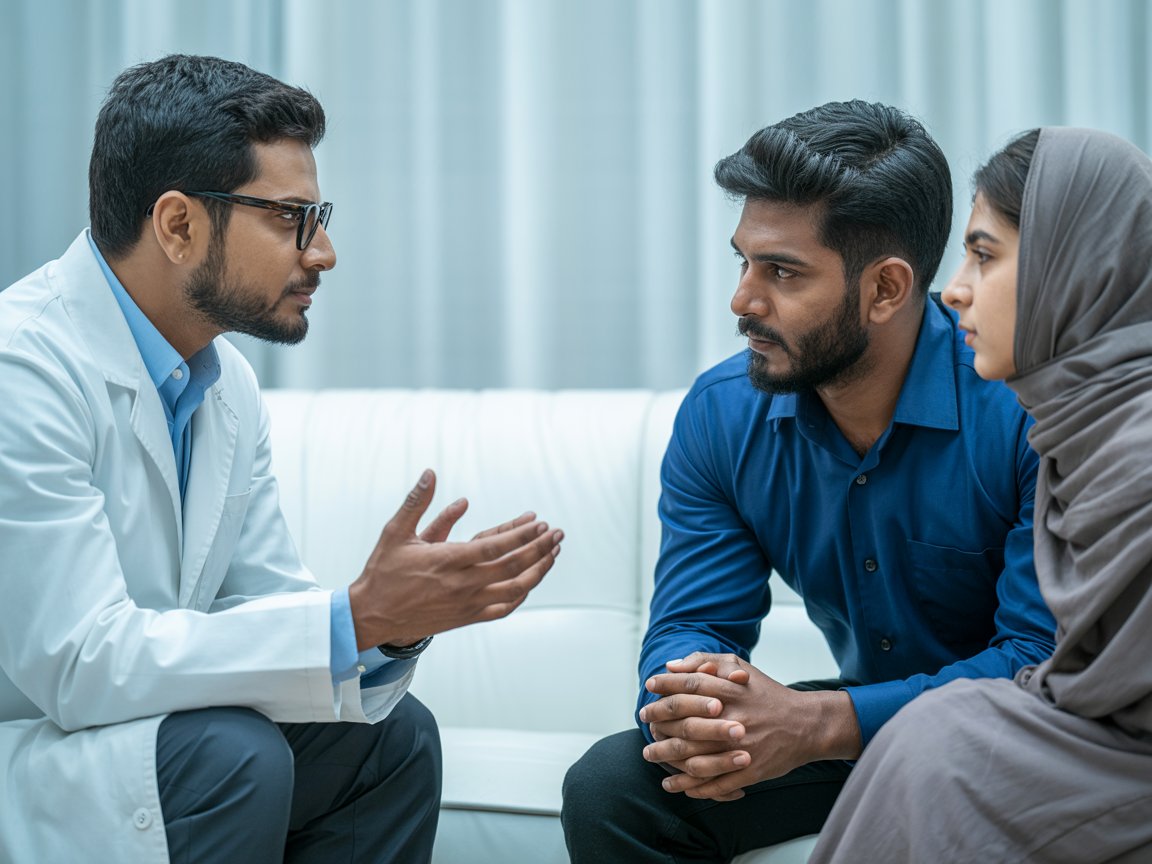





First of all Congratulations. Very well written. Secondly, the article shows the empathy of doctors as well. Very often we come out of seeing a doctor with the feeling that the doctor was all clinical and perhaps did not realise the suffering one is going thru. But it also true that in India, the rush of patients is such the doctors have very little time for anything other than providing clinical services. However, if the doctor does empathise it goes a long way in psychological healing. Thirdly the pain & suffering of the patient side is well captured. Dr Sarath has all the hallmarks of being a great healer.